Thyroid surgery, also known as thyroidectomy, is a medical procedure performed to remove all or part of the thyroid gland. This surgery is necessary in cases such as thyroid cancer, large benign nodules causing discomfort, hyperthyroidism, or goiters. Understanding the process, risks, and recovery involved in thyroid surgery can help patients feel more prepared and informed. This blog will provide an overview of the types of thyroid surgeries, the reasons for undergoing surgery, the procedure itself, and the recovery process.
What Is Thyroid Surgery?
The thyroid is a butterfly-shaped gland located at the base of your neck, responsible for producing hormones that regulate your metabolism, heart rate, and body temperature. Thyroid surgery is typically recommended when there are problems with this gland, such as:
- Thyroid Cancer: If cancerous cells are detected in the thyroid, surgery is often the most effective way to remove the tumor.
- Nodules or Cysts: Sometimes, nodules or cysts on the thyroid can grow large enough to cause discomfort or difficulty swallowing and breathing, even if they aren’t cancerous.
- Hyperthyroidism: This condition occurs when the thyroid produces too many hormones, and in cases where other treatments fail, surgery may be an option.
- Goiter: A non-cancerous enlargement of the thyroid gland can cause compression in the neck, leading to problems with swallowing or breathing, requiring surgical intervention.
Types of Thyroid Surgery
There are several types of thyroid surgeries, depending on the condition being treated and the extent of the problem:
-
Total Thyroidectomy: This involves the removal of the entire thyroid gland. It is usually done in cases of thyroid cancer or severe hyperthyroidism.
-
Partial Thyroidectomy (Lobectomy): Only part of the thyroid gland is removed, typically in cases of benign nodules or hyperthyroidism. The remaining part of the thyroid often continues to function.
-
Subtotal Thyroidectomy: In this procedure, most of the thyroid gland is removed, leaving behind a small portion of the tissue. It’s often performed to treat hyperthyroidism or large goiters.
The choice of surgery depends on factors like the severity of the condition, the presence of cancer, and the overall health of the patient.
The Thyroid Surgery Procedure
Thyroid surgery is typically performed under general anesthesia and usually lasts between one to two hours, depending on the type of surgery. Here is a step-by-step outline of what to expect:
-
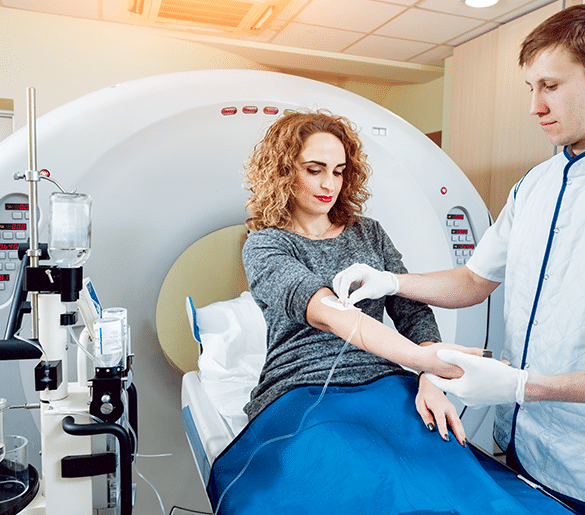
Preoperative Preparation: Before surgery, the patient will have a pre-surgical consultation, including a physical examination, blood tests, and sometimes imaging tests like an ultrasound or CT scan. Your surgeon will explain the procedure and the risks involved.
-
During Surgery:
- A small incision is made at the front of the neck.
- The surgeon carefully works to avoid damaging surrounding structures, including the parathyroid glands (which regulate calcium levels) and the recurrent laryngeal nerves (which control the vocal cords).
- Depending on the type of thyroidectomy, part or all of the thyroid gland is removed.
-
Post-Surgery: After the surgery is completed, the incision is closed with stitches or surgical glue. In some cases, a small drainage tube may be placed to remove excess fluids.
Risks and Complications
Like all surgeries, thyroid surgery comes with potential risks, though they are rare. Some of the possible complications include:
- Damage to the Vocal Cords: The recurrent laryngeal nerve runs close to the thyroid, and any damage to it could affect the voice. Hoarseness or a weaker voice is possible but usually temporary.
- Hypoparathyroidism: Damage to the parathyroid glands can lead to low calcium levels in the body, causing tingling, muscle cramps, or spasms.
- Infection or Bleeding: As with any surgery, there is a small risk of infection or excessive bleeding.
- Hypothyroidism: If the entire thyroid gland is removed, the body can no longer produce thyroid hormones, leading to hypothyroidism. Patients will need lifelong thyroid hormone replacement therapy.
Recovery After Thyroid Surgery
Recovery from thyroid surgery is generally smooth, but the time it takes to fully recover depends on the extent of the surgery. Here’s what to expect:
-
Hospital Stay: Most patients stay in the hospital for one to two days following surgery, but in some cases, it may be an outpatient procedure.
-
Incision Care: The incision site may be slightly sore for a few days. It is important to follow the surgeon’s instructions on how to care for the incision to avoid infection and minimize scarring.
-
Pain Management: Mild pain or discomfort can be managed with over-the-counter pain relievers. Most patients report only minimal discomfort after the surgery.
-
Voice Changes: Some patients may experience temporary hoarseness or a change in voice pitch due to swelling around the vocal cords. This typically resolves within a few weeks.
-
Return to Normal Activities: Most people can resume normal activities, such as walking or light tasks, within a few days, but heavy lifting or strenuous activities should be avoided for a few weeks.
-
Follow-Up: After surgery, a follow-up visit with your surgeon is necessary to monitor the healing process and check for any complications. In the case of total thyroidectomy, your doctor will likely prescribe thyroid hormone replacement therapy, which you will need to take for life.
Life After Thyroid Surgery
For most patients, life after thyroid surgery is manageable and often leads to an improved quality of life. However, it is important to:
-
Monitor Hormone Levels: If you’ve had a total thyroidectomy, your doctor will prescribe thyroid hormone pills to replace the hormones your thyroid used to make. Your doctor will periodically check your hormone levels to make sure you’re getting the correct dosage.
-
Calcium Monitoring: If the parathyroid glands were affected during surgery, your calcium levels may need to be monitored. Calcium supplements may be prescribed if necessary.
-
Diet and Lifestyle: There are usually no major dietary restrictions after thyroid surgery, but maintaining a healthy diet and lifestyle can help with recovery and long-term health.