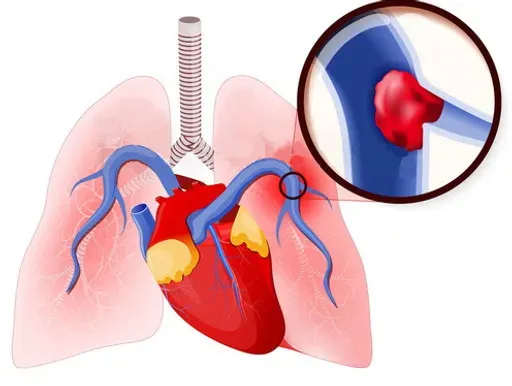
A blockage in one of the pulmonary arteries in your lungs might result in a pulmonary embolism (PE), a dangerous medical illness. Blood clots that migrate from other regions of the body, especially the legs, to the lungs are frequently the cause of the blockage. Early detection of pulmonary embolism symptoms can save lives and is essential for timely treatment. This article will discuss pulmonary embolism symptoms, risk factors, diagnostic techniques, and prevention strategies.
What is Pulmonary Embolism?
Pulmonary embolism occurs when a blood clot, known as a thrombus, obstructs blood flow in the lungs. This can lead to reduced oxygen levels in the blood and damage to lung tissue. Left untreated, PE can be life-threatening, but timely intervention can significantly improve outcomes.
Common Symptoms of Pulmonary Embolism
Symptoms of pulmonary embolism can vary in severity depending on the size of the clot and its location. Some common signs include:
- Shortness of Breath:
- Sudden onset of difficulty breathing is the most common symptom of PE. It can occur at rest or during physical activity.
- Chest Pain:
- Sharp, stabbing pain in the chest that worsens with deep breaths or coughing.
- Coughing (Sometimes with Blood):
- Persistent coughing, often accompanied by bloody or pink-tinged sputum.
- Rapid Heartbeat (Tachycardia):
- A noticeably fast or irregular heartbeat.
- Dizziness or Fainting:
- Feeling lightheaded or losing consciousness due to reduced oxygen flow.
- Leg Swelling and Pain:
- Swelling, redness, or cramping in the legs, particularly in the calf or thigh, indicating a deep vein thrombosis (DVT).
- Bluish or Pale Skin (Cyanosis):
- A bluish tint on the skin due to inadequate oxygen levels.
Risk Factors for Pulmonary Embolism
Certain factors can increase your risk of developing PE:
- Prolonged Inactivity:
- Extended periods of immobility, such as during long flights or hospital stays.
- Surgery or Trauma:
- Post-surgical recovery and injuries that impair blood circulation.
- Medical Conditions:
- Conditions like cancer, heart disease, or clotting disorders.
- Pregnancy and Postpartum Period:
- Hormonal changes during and after pregnancy can heighten the risk.
- Lifestyle Factors:
- Smoking, obesity, and sedentary behavior can contribute to blood clot formation.
When to Seek Medical Attention
If you experience symptoms of pulmonary embolism, particularly severe shortness of breath, chest pain, or coughing up blood, seek medical attention immediately. Delayed treatment can lead to serious complications, including permanent lung damage or death.
Diagnosis and Treatment of Pulmonary Embolism
Diagnosing pulmonary embolism involves a combination of tests and medical evaluations, such as:
- Blood Tests:
- To detect clotting abnormalities and measure oxygen levels.
- Imaging Scans:
- CT pulmonary angiography or chest X-rays to visualize blockages in the lungs.
- Ultrasound:
- Used to detect deep vein thrombosis in the legs.
- Electrocardiogram (ECG):
- Helps rule out other conditions, such as heart attacks.
Treatment Options Include:
- Anticoagulants (Blood Thinners):
- Medications like heparin or warfarin to prevent clot growth and new clots from forming.
- Thrombolytics:
- Drugs to dissolve large clots in emergency situations.
- Surgery or Catheter Procedures:
- In severe cases, clots may be removed through surgical interventions.
Preventing Pulmonary Embolism
Prevention plays a vital role in reducing the risk of pulmonary embolism. Here are some actionable tips:
- Stay Active:
- Regular physical activity, especially after surgery or long travel, helps improve circulation.
- Wear Compression Stockings:
- Useful for individuals at risk of deep vein thrombosis.
- Maintain a Healthy Lifestyle:
- Avoid smoking, maintain a healthy weight, and follow a balanced diet.
- Take Prescribed Medications:
- Follow your doctor’s instructions if you are prescribed anticoagulants.
- Stay Hydrated:
- Drinking water prevents dehydration, a factor contributing to blood clot formation.
FAQs about Pulmonary Embolism
Q1: Can pulmonary embolism occur without symptoms?
Yes, small clots may not cause noticeable symptoms but can still pose a risk. Regular check-ups are important for at-risk individuals.
Q2: How quickly does pulmonary embolism develop?
PE can develop suddenly, often within hours or days, especially after surgery or prolonged immobility.
Q3: Is pulmonary embolism hereditary?
Certain genetic conditions that affect blood clotting, like Factor V Leiden, can increase the risk.
Q4: What should I do if I suspect I have a pulmonary embolism?
Seek emergency medical care immediately if you notice severe symptoms like chest pain, shortness of breath, or fainting.
Q5: Are there long-term effects of pulmonary embolism?
Yes, untreated PE can lead to chronic conditions like pulmonary hypertension or recurrent clots.
Conclusion
Recognizing the symptoms of pulmonary embolism early is critical for timely intervention. Understanding the risk factors and implementing preventive measures can help reduce the likelihood of this life-threatening condition. Stay informed, and consult your healthcare provider for personalized advice to manage your health effectively.
By staying vigilant and proactive, you can safeguard yourself against the dangers of pulmonary embolism.